Episode 356
For many of us, agency ownership means that most of our time and energy goes into our work. Even when trying to sleep, we’re replaying a frustrating conversation we had earlier that day, doomscrolling, or even dreaming about everything on our to-do lists. When we can’t turn off our minds at the end of a long day, we set ourselves up for occupational burnout.
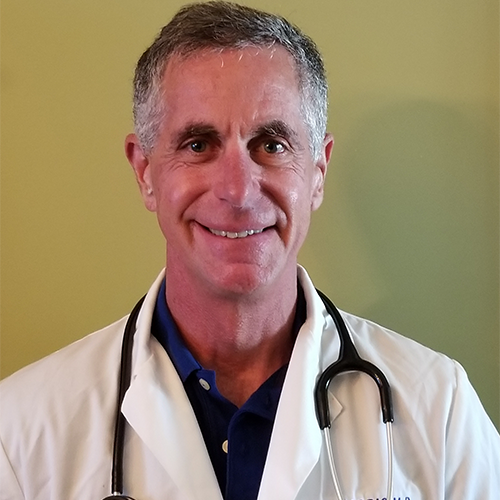
As some of you know, I learned the hard way that staying overly connected to our work can have severe consequences. I brought Dr. Gerry Farris on the podcast today to talk about how we can take care of ourselves to feel better daily, stay mentally strong and healthy, and why taking breaks is so important. With many years as a physician and working with patients who have experienced occupational burnout, Dr. Farris is the perfect person to educate us on how to be smarter about living our overly-connected lives.
Dr. Gerry Farris has been an Emergency physician for 30 years and a Functional Medicine physician for 10 years. His current practice focuses on healthy living and age management and he is a former triathlete who competed for 31 years. His goal is to help patients and persons be healthy, mitigate disease and aging, and live well for a long time. He is a double Board Certified physician with a wealth of experience and knowledge. He is practicing the “Medicine of Tomorrow, Today!”
A big thank you to our podcast’s presenting sponsor, White Label IQ. They’re an amazing resource for agencies who want to outsource their design, dev, or PPC work at wholesale prices. Check out their special offer (10 free hours!) for podcast listeners here.

What You Will Learn in This Episode:
- How to know if you’re experiencing occupational burnout or heading in that direction
- How information overload leads to hypervigilance and why it happens
- The effects that elevated cortisol levels have on our brains and bodies
- How to build resilience against neuroinflammation and bodily dysregulation
- What does burnout recovery look like?
- Why sleep is one of the most essential things for recovery and burnout prevention
- What 37 minutes a day can do to improve your overall health
- How to make healthy lifestyle changes that you can stick to
“I don't think we have quite adapted as a species to the amount of information overload that we're being exposed to.” Dr. Gerry Farris Share on X“We have to understand that if we are going to live the lifestyle we're going to live, we want to live, and have to live in certain cases, that we have to now allocate time for ourselves for recovery.” Dr. Gerry Farris Share on X“We give away our time. We don't honor our own time when we need to honor our own time. We don't get enough downtime.” Dr. Gerry Farris Share on X“We found that we should not work more than three days in a row because of the decline in performance. If we work three-twelves or three-sixteens, it drops off the cliff. We found this out within the first month.” Dr. Gerry Farris Share on X“So what I'm really preaching to you is let's work on being better men, women, and leaders by taking care of ourselves.” Dr. Gerry Farris Share on X
Ways to contact Dr. Gerry Farris:
- Website (practice): https://www.gefarrismd.com/
- LinkedIn (personal): https://www.linkedin.com/in/gerry-farris-23a1535b/
Resources:
Speaker 1:
If you’re going to take the risk of running an agency, shouldn’t you get the benefits too? Welcome to Agency Management Institute’s Build a Better Agency Podcast, presented by White Label IQ. Tune in every week for insights on how small to mid-size agencies are surviving and thriving in today’s market. We’ll show you how to make more money and keep more of what you make. We want to help you build an agency that is sustainable, scalable, and if you want down the road, sellable. With 25-plus years of experience as both an agency owner and agency consultant, please welcome your host, Drew McLellan.
Drew McLellan:
Hey, everybody, Drew McLellan here from Agency Management Institute. We have a great episode for you today. I’m going to tell you why I think it’s so important in a minute. Super excited about it. And I think it’s going to be something that you think about for a really long time. But before I do that, let me tell you, we just finalized working out with our friends at Mercer Island Group, the brand new workshop that they’re going to do in January of 2023, which seems so far away, but the reality is it’s only six, seven months away.
Here’s what they’re going to do is they are going to teach us for two days all of the ways that we could improve our written proposals. So, that could be something where somebody has a referral and they just ask you to write a proposal without sending out any information to maybe have a discovery call or a discovery meeting. And then, they ask you to give them a proposal. It could be anything as formal as a response to an RFI or an RFP.
We’re going to talk about case studies and cover letters, and we are going to workshop some of it. So, you can actually learn how to do it better. And then, we’re, for two days, just going to immerse ourselves in how to make our proposals more successful. How do we increase our win rate? So, that workshop is going to be at the tail end of January in Orlando. By the time this episode airs, it will be on the website.
So, if you want to learn more about it and see the dates and all of that thing, head over to agencymanagementinstitute.com, and under the How We Help tab, you scroll down to Workshops and it’ll be there. So, check that out and don’t miss it because I think it’s going to be awesome. All right. So, I’m going to tell you a little story and some of you were a part of this story, so you’ll recognize it. And others of you, it’ll be new news.
So, life in spring of 2022 for me was really great in a lot of ways, a lot of really good, happy life things happening, but also had some family losses and some family illness and then we’re planning the summit. And there’s just some stressors like all of you have. And I will admit, I have a tendency to be a bit of workaholic.
So, I work a lot of hours and I don’t take a lot of time off on the weekends and I carve time out. I will spend time with family and friends for a couple of hours or a half a day, but I am always going a hundred miles an hour. I suspect you recognize yourself in that description. A lot of you are wired a lot like I am. So, it is the summit, we are in Chicago. We have 300 attendees. We have all these sponsors.
I’m feeling incredible pressure to make that experience as amazing as possible for everyone. Have some family stuff going on at the same time that I’m also worried about. So, I’m feeling very fragmented. And so, on Monday, Monday of the summit is what we call Family Days. So, it’s basically for all of the members who are in attendance. We have a half day of learning together, speakers, panels, things like that. And then, we go to dinner.
And it’s such a great day. I’m with 150 people that I know really well that I genuinely love. I am so excited to be with all of them, but I also have to be on. I’m on stage a lot. I’m the conductor of the orchestra, if you will. So, that particular Monday, which was a couple of months ago now, I didn’t do a very good job of taking care of myself. I didn’t get a good night’s sleep the night before. I was not staying as hydrated. I was so scattered and stretched.
I didn’t eat very well that day. And again, I’m on. So, I’m high energy the entire day. There’s stuff going on at home that I’m trying to keep track of. And again, a lot of good things, but also a lot of stressful things. So, for many of you, this is like your normal life. Like it’s my normal life. Well, anyway, so the day is really great. We have great panels. Everybody’s feeling high energy. We all go to dinner.
And I’m walking the room. Everybody’s seated for dinner and I’m walking the room, talking to people, almost like, you’re the host of a wedding. That’s what it felt like to me. Like I wanted to make sure I said hi to everybody and saw everybody and hugged everybody. And finally, somebody said, “You know what? You need to sit down and eat.” So, I sat down and I passed out, and I could feel myself getting so lightheaded. I passed out and I hit my head really hard on the floor.
Long story short. So, here I am in front of 150 of my friends who are clients, freak them all out. They call the paramedics, cops come. It was awful. And then, I had the summit still. So, long story short, I stayed in Chicago. I was present at the summit. I gave my keynote, but I felt really lousy. Whenever I didn’t have to be on stage or in front of everybody, I was in my hotel room sleeping, and I felt bad.
I just didn’t feel good. So, I had a headache and I was nauseous and I didn’t get sick or anything like that. So, we were assuming that there was no concussion, but when I got home, my family insisted that I go see a doctor. And long story short, I did have a concussion and it took me six weeks to really recover from that concussion. I slept all the time. It really reduced my screen time because I had to. I just didn’t feel good.
And I now finally am feeling full of energy again, feeling strong, feeling healthy. And I’m telling you all of this because our lives are pressure cookers. And what happened on that Monday night was my body said, “We’ve been trying to get your attention. We’ve been trying to tell you to slow down. We’ve been trying to tell you to not work so much. We’ve been trying to tell you to manage your stress. We’ve been trying to tell you to drink more water and eat healthier and all the things.”
And I, of course just kept pushing and pushing and pushing because I have obligations and I want to do right by everybody and all the things, all the reasons that we give every day these excuses that we give. And at a certain point in time, my body said, “Okay, I’ve thrown a pebble at you. I’ve thrown a rock at you. I’ve thrown a boulder at you. Apparently, I’m going to need to hit you with a mountain and I’m going to need to just knock you on your rear end, literally knock you on your rear end and knock you out to get your attention.”
And that’s exactly what happened. I hope for most of you, you haven’t pushed yourself to that extreme, but I know you all push yourself every single day. I know that you don’t eat as well as you should. I know you work too many hours. Especially right now, I know that many of you are feeling this weight that you can’t quite articulate what it is or why it is, but you feel this heaviness.
And a lot of you have said to me, “I just can’t get my mojo back. We can back after COVID, the business is fine, but I just can’t. I can’t get my enthusiasm back. I can’t get my energy back.” And so, that’s what today’s guest is all about. Dr. Gerry Farris is an ER doc. He is a specialist in all medicine, but particularly this idea of what is holistic integrated medicine when it comes to what we’re doing to ourselves in this high-stress world that we live in.
And what do we do to balance all of the things, all the pressures that we’re putting on our body, and what are the consequences if we don’t do anything? So, I have a very personal vested interest in this topic because of what’s happened lately. And I have a very vested interest in this topic because I talk to all of you every day, and I hear your stress and your frustration and your short-temperedness and your lack of joy around the work.
And so, I really want Gerry to talk to us about how we take better care of ourselves, how we manage in this stress, pressure cooker world that we live in so that we don’t pass out in front of 150 clients. And we don’t trigger other health issues that have consequences much bigger than we want to deal with. So, that’s what this is. So, I want to get right to it.
I want to introduce you to Gerry and have him tell us what’s going on in our bodies when it manifests itself in the ways that we’re all seeing. All right. So, let’s do it. Gerry, welcome to the podcast. Thanks for joining us.
Dr. Gerry Farris:
Thank you, Drew. It’s really exciting to be here.
Drew McLellan:
The topic of burnout and all the stress that business owners and other business people are under is such a hot topic. I can’t wait to dig into this with you, but before we do that, why don’t you tell the listeners a little bit about your background and how you came to have this depth of expertise?
Dr. Gerry Farris:
Absolutely. So, folks, the reason I do the work I do is because I went through some of the things and at the time I went through it, there was no answers. What do they say, when you want to find the solution to a problem, you have to go through it yourself. To give you my background, I’ve been a physician for now, 30 years. I have been an ER doctor for 30 years.
Drew McLellan:
Yeah. There’s a little source of burnout, I bet.
Dr. Gerry Farris:
Yeah. So, I’ve done my share of nights and weekends and holidays and chaos and COVID and all of that good stuff. Also, I aspired to be a masters athlete. So, I was a triathlete for 31 years. And I actually had the honor to race on US team at one time as a masters athlete. And that was another reason I became very familiar with burnout is when you’re trying to train as an athlete and raise a family and work as a doctor, I can tell you something gibs.
So, what I’m going to try to take you all through is really part of my experience because when I went through it 20 years ago or so, nobody had any answers. You go see somebody and they’re just like, “Well, I don’t know what to tell you. I’ll put you on antidepressant.” I’m like, “I don’t need an antidepressant. I need a solution to the problem.” So, this embarked me into the world of now what we call functional and integrative medicine, which I’ve been practicing for the last 12 years.
What that really entails is this idea of how do we really be health, how do we take care of ourselves? Because I can tell you working in healthcare, the healthcare system is a disaster. We know it. And I always bring this up, this is salient, this is less about me, but we spend so much more per patient in the United States on healthcare yet our health outcomes are pitiful.
My mantra now is we’re trying to teach people, how do you be healthy? How do you live this life at warp speed? And we’ll get into this. We’re having to live at warp speed.
Drew McLellan:
Right. Every day.
Dr. Gerry Farris:
Whether it’s self-induced or just societal-induced or whether it’s just the lifestyle we lead. As we talk about this topic, you’ll see where I’m going with this. So, again, 30 years as a doctor, 12 years doing this practice of integrative medicine, trying to help people be healthy, former athlete, been through it, done it, seen it, and now, what we’re really working on is how do we help others?
Because physician burnout is huge, and I’m involved in a research study with it right now. So, this is where all this becomes very timely. And all I’m going to do is translate the same information to your listeners today.
Drew McLellan:
Yeah. That’s awesome. I’ve been doing this work for a really long time and it’s always been a pressure cooker job, but certainly, the last several years have taken a tremendous toll on the folks that are listening to this podcast and that we get to work with, just in terms of feels like there’s never a letup. There’s always more of a thing. So, let’s talk a little bit about burnout and how does somebody know if they are burnt out? What does it look like? What does it feel like?
Dr. Gerry Farris:
Again, one of the big things you start to see is this overwhelming sense of fatigue. And most of us are all type A, AA, AAA personalities. And our whole mantra through life is we’re just going to power through. And it’s this, I’m fatigued, now I’m not sleeping well, I’m not rested when I’m sleeping. And then, it starts to move into the irritability phase.
Then we start to get irritable with our loved ones and we get irritable and we snap, and we have very short tempers with our coworkers and little things set us off. So, we start to build this pattern and, “Well, Dr. Farris is always on edge. Why is he always on edge?”
Drew McLellan:
Which I think a lot of agency owners, they’re hearing that from their employees, like, “You’re always on edge or I’m anxious to even come talk to you because I already know it’s going to escalate.” And nobody wants to show up that way.
Dr. Gerry Farris:
No. So, again, fatigue, sleep dysregulation, and we really going to hit on that hard. And then, we can really take it further because I can now run certain laboratory tests on you to show you where you are in life. So, we can start to do the diagnostics and look under the hood, not like what your doctor’s doing. Where we can really look under the hood and go, “Well, gee, Drew, this is what your body’s telling you.”
And then, what we’ll get into later is this idea of biometric monitoring, which is now becoming a very fascinating piece of it, where I can monitor myself day to day or week to week and start to see where my patterns are. Am I getting worse? Am I getting better? So, that’s the broad how does that happen.
Drew McLellan:
So, has burnout always been a thing, or is this a modern phenomenon do you think?
Dr. Gerry Farris:
I really think that this is much more of a modern phenomenon, and I’ll tell you why. Now, if you look at us from an evolutionary standpoint, we were mostly in the beginning hunter-gatherers, and then we became industrialized. So, we were still either farmers or factory workers, and we did more manual labor. There were still the cerebral people.
There were still the leaders that did more of the cerebral work. But we’re in a pretty simple society up through the ’60s, ’70s and early ’80s. And then, we had the advent of computers, data, input, and just the accessibility to constant information.
Drew McLellan:
And more information than we could possibly consume.
Dr. Gerry Farris:
And then, it’s addicting. It’s addicting. So, what ended up happening is, I don’t think we have quite adapted as a species to the amount of information overload that we’re being exposed to. And we can take this further and talk about EMF and I’m happy to discuss all these things, but the point is, we’re getting just so much data all the time. And what do you process? Because the brain wants to process everything and you got to kick in what’s important which is not important. So, we start to move into this idea that we call hypervigilance. I need to expound on hypervigilance a little bit. Okay?
Now, we need to be aware of things going on. Obviously, if you go into a new city, you don’t know the area, you’re vigilant. Because you don’t want to go down the wrong street. You don’t want to go on the bad area of town. So, that’s vigilance where it’s good. But the brain doesn’t know when we start to get exposed to all this data, what do I really need to be paying attention to? We don’t put the filters on.
So, now, we stay in this constant state of upregulation of something called cortisol, which is a really important stress hormone. We have overload of epinephrine and some of these neurotransmitters because we’re now being forced to run at a processing speed that is much higher than we were maybe ready for.
I don’t know if this resonates with your listeners, but this is what we began to see. I saw this as an athlete when I started to overtrain. It’s the same idea. It’s, how are we adapting to the stimulus that’s being placed on us.
Drew McLellan:
Well, and you’re right. With our phones and all the other ways we can get information, nobody ever unplugs really. It’s always on. My daughter used the phrase the other day, doom scrolling, where you are just caught in this perpetual loop of reading bad news. To some extent, we’re all doing that.
Dr. Gerry Farris:
Right. In my work, when clients come to see me, I always ask them this question, what is the first thing you do in the morning? What is the last thing you do before you go to bed? Now, I get it. But at some point, we have to give our brain a rest. And when we don’t give our brain a rest and we don’t recover, we start to create this problem called neuroinflammation.
And we got to talk about neuroinflammation because neuroinflammation, and I will tell you, is what goes on to create diseases that we don’t want to talk about. That’s the Alzheimer’s and the Parkinson’s and some mental illness as well. So, we’re not shutting off. We’re just not shutting off.
Drew McLellan:
So, how do we shut off? We can all talk about putting down a phone or whatever. But to your point, we are moving at hyper-warp speed. That’s not going to slow down if anything is going to pick up. So, how do we build resilience and how do we take better care of ourself?
Dr. Gerry Farris:
Incredibly great question. And that’s what we’re going to jump into now. Because part of this when I originally did this, the title of the talk was What Are You Doing to Your Brain and What Are You Doing for Your Brain? And I got asked a lot of questions about what are we doing to our brain. Again, we’ve started to touch on it. And then, they said, “What do you mean, I’m supposed to be doing something for my brain?”
Well, think about it. We go to the gym, we lift weights. That’s good for us. But do we put any effort into the care of one of the most important parts of our body. I need everybody to think about this just for a moment and just soak it in. We’re asking the engine to really push really hard yet we don’t want to rest the engine. And then, we wonder why the engine starts to have knocks and pings and then goes on to have problems. So, this is the path where I want to go.
So, first of all, we have to understand that if we are going to live the lifestyle we want to live and have to live in certain cases, that we have to now have allocated time for ourself to recovery. And this is where we’re starting to really get into trouble, is we’re not allocating enough recovery time, which is where we get sleep dysregulation. We get what’s called hypothalamic-pituitary axis or adrenal dysregulation.
This is elevated cortisol, which starts to really affect the brain. I don’t want to get too deep into the science, but there starts to be deleterious effects to the body, the brain, the emotions, the spirituality, if we are not actively spending time in some recovery mode.
Drew McLellan:
And what does recovery look like?
Dr. Gerry Farris:
It looks like walks in the woods. It looks like meditation. And I know we don’t want to do meditation. It looks like spending time doing nothing. It looks like really going to sleep at night and sleeping through the night, checking out of the things that are really not important in our life, filtering. Don’t need to be on Facebook. Don’t need to be on Instagram.
Drew McLellan:
Or at least not for three hours a day.
Dr. Gerry Farris:
This is really important. They have done early studies on teenagers and they’re starting to see neuroinflammation from information overload. And we’re talking about teenagers. This is unheard of, Drew.
Drew McLellan:
This is, if we don’t model this, our kids are really in trouble because they’ve grown up with the information overload. Most of us, it came into our life at some stage of either early adulthood or whatever. But our kids don’t know any different.
Dr. Gerry Farris:
No, this is their life. And again, there may be a little bit more adaptive than we were. I’m 61, so I didn’t grow up with this. If we’re not adapting correctly, there’s going to be a problem. So, part one is we have to start to allocate me time. We give away our time. My wife reminds me about all the time. We give away our time. We don’t honor our own time when we need to honor our own time. We don’t get enough downtime.
Drew McLellan:
I know somebody’s listening, going, “Okay, what is enough downtime?” Like what’s the minimum amount I can… because I’m hearing their questions. What’s the bare minimum I can do to be more resilient and to recover? What does that look like?
Dr. Gerry Farris:
That’s 10 and 20-minute breaks during the day. That’s eight hours of sleep at night. There’s your bare minimum. But we cannot continue to work 16 hours a day, get five hours of dysregulated sleep, eat a garbage diet and expect to run like a Porsche. It’s just not going to work. Resiliency is going to catch up with you. And back to the original point, we can power through up to a point.
Drew McLellan:
And then, your body takes over and says, “You’re not listening so I’m going to show you.”
Dr. Gerry Farris:
And this is where I want to go with this. So, this idea of cortisol, cortisol being the stress hormone, again, very important if somebody’s holding a gun to you but becomes deleterious to us when we’re constantly stressed all the time. Because when the cortisol level goes up over a long period of time, it starts to affect the brain. It can actually start to shrink and damage two areas of the brain. Now, where am I going with that, doc?
Well, I’m going to tell you, okay? Your body is very, very smart. When you start to injure the brain, it’s going to shut you down. And this is the end stage that we start to see where all of a sudden, you go from a functioning CEO to, I can’t get off the couch and I don’t know what happened to me.
Drew McLellan:
Or I just can’t shake the mood. I just can’t get out of this mood. It’s not a day. It’s not a week. It’s just, I can’t. I have this feeling of dread or doom or weight that I cannot get rid of.
Dr. Gerry Farris:
100%. There you are. Now, we’ve reached and that’s I’m here to talk about. So, we don’t get into end stage because once you start to get to that level where we’re way down the rabbit hole, even in an expert’s hands, it’s going to take a lot of time. So, this is back to, an ounce of prevention is better than a pound of cure, because it’s more than a pound of cure.
Drew McLellan:
All right. I want to talk about some of the things that we need to do to begin to combat this, but let’s take a quick break and then let’s talk about some really pragmatic, practical things that people can weave into their daily lives so that they can protect themselves from that end stage of burnout. So, let’s take a quick break and we’ll come right back. Hey, I promise we will get right back to the conversation, but I wanted to make sure you knew that we have two AE Bootcamps coming up, two live workshops.
The first one is the Advanced AE Bootcamp. That’s going to be for folks who have five years or so of experience being an AE in an agency. That’s going to be in Chicago, June 16th and 17th. And you could register by going to the AMI website and going under the How We Help and finding the Workshop tab. And you’ll find the Advanced AE Bootcamp there. So, again, it’s two full days of learning and sharing.
So, the AEs not only learn from us, the instructors, but they also learn from each other throughout the workshop. So, we get rave reviews and it’s a great way for your AEs to really level up and become a leader inside your organization. So, again, June 16th and 17th for the Advanced AE Bootcamp. And then, August 1st and second, the Regular AE Bootcamp.
So, that’s going to be for folks with less than five years of experience, account coordinators, project managers, AEs, anybody who is new into their career and still trying to figure out what the AE thing is all about. Honestly, it’s about helping them understand that they need to move from being an order taker to helping grow your client’s business and growing the agency’s business. So, again, August 1st and second, also in Chicago. Hopefully, we’ll see some of your folks there.
All right, let’s get back to the conversation. All right. I am here with Dr. Gerry Farris and we are talking about burnout and the consequences of burnout, which I don’t know about you, but the first 20 minutes have me freaking out a little bit. I don’t know about you guys, but I’m certainly recognizing some of the things he’s talking about, showing up in my life now and then. And I can’t think of any of you, and I hang out with you guys all the time.
I cannot think of any of you where you can’t be feeling some of this fatigue and frustration and irritation and the irregular sleep and all the other things that Dr. Farris has been talking about. All right. Let’s say we recognize ourselves in your descriptions. What do we do?
How do we still function and do our work and have time with our family and do the volunteer, whatever the things are? We want to have the life, as you said, we want to live the life we want to live. How do we do that but also protect ourselves better than it sounds like we are?
Dr. Gerry Farris:
Got it. One, again, you talked about it. The first thing is acknowledge the problem. So, you have to acknowledge that you can’t live in the dark on it. So, we have to do the acknowledgment of it. Then we have to start to come up with what is the best plan for that person based on where they are in life. Now, we know the following things that I will discuss are all pertinent for everybody. It’s just, to what degree do we turn the knob one way versus the other? So, let’s start with the most important thing in my mind and that’s sleep.
Drew McLellan:
And probably something we all abuse.
Dr. Gerry Farris:
Because again, I’ve been an ER doctor a long time. They would let me work 25 hours in a row if they could get away with it. We know it’s not safe that it’s not healthy, but that’s the world we live in. So, sleep could be one of the most critical things you do and not just sleep, real sleep. Because we think we’re sleeping. Are we dreaming? Are we getting into the deeper stages of sleep, which is REM and slow-wave sleep such that now the body can repair itself and the brain can repair itself?
Now, that became important when we started to look at the biometrics of the WHOOP, because when you wear a wearable and again, for people, this can be a really eye-opening experience is to put on one of these things and monitor yourself and see. Well, I laid in bed eight hours and I got about four hours of light sleep and little to no REM or slow-wave sleep.
Drew McLellan:
And why would that be?
Dr. Gerry Farris:
Again, still we can’t shut our brain off. I’ve got this meeting tomorrow. I’ve got to sign this contract. I’ve got to do this presentation. We go to bed thinking about it.
Drew McLellan:
Wake up in the middle of the night thinking about it.
Dr. Gerry Farris:
The subconscious is just running wild. And thus, we don’t get into the deeper stages of sleep. When you go to your doctor, what happens? You get put on Ambien or you get put on trazodone or benzodiazepine, and we can go down the list of all the medications for sleep. And those do put you to sleep. They never get you into deep sleep. More importantly, and I really want to hit home with this, long-term use of these medications will lead directly to cognitive decline.
And I spend a lot of my time and I don’t mean to scare people, but when you see these guys and girls been on all these sleep medications forever and the brain fog. So, we have to work on, can we do natural things to help us sleep? Can we decompress? Can we turn the computer off a few minutes early? Can we go to bed earlier?
Can we take some magnesium or some melatonin or some natural sleep aid? And can we start to slow ourselves down?” So, we don’t put the laptop away and then go, “I’m going to go to sleep now.” We all do it.
Drew McLellan:
Everybody just recognized themselves. Everyone just went, “Oh crap, he just called me out on that.”
Dr. Gerry Farris:
And I’m not calling you out.
Drew McLellan:
But it’s the truth. It’s right.
Dr. Gerry Farris:
Right. So, we start to adapt, what are we going to do for sleep hygiene? We got to make sure our room is cold. We got to make sure our room is dark. Maybe some simple stretching. Just read a book, do something where we start to calm the mind, calm the mind a little bit so that we can start to get into this better sleep. And again, the monitoring of sleep has been, and again, this study, I wish they would let me publish what I want to publish, but it’s groundbreaking. It was just groundbreaking looking at physicians.
We found that we should not work more than three days in a row because the decline, and this is salient for your people, are decline in performance. If we work three-twelves or three-sixteens, it drops off the cliff. We found this out within the first month. We couldn’t believe it. We didn’t know what to expect. We’re just running the experiment.
And your listeners, they’re working six-plus days a week, trying to manage everything. And if you got decline at three, what happens at four, five, and six? And then, you don’t recovery. How do you bring you’re A game the following week?
Drew McLellan:
Well, and how do you not continue to cause more and more damage if you never let up?
Dr. Gerry Farris:
Right. So, again, sleep would be critically important. Diet becomes critically important. And again, I’m not telling anybody to go on a diet. I’m telling you, we have to learn to fuel the body correctly. And that’s what I’m talking about. We have to get away from some of these processing foods. We have to eat more naturally. So, when people come in and say, “Well, how should I eat, doc?” I tell them to eat like a farmer. Because what does farmer eat? If you can’t grow it, kill it, pick it. You can’t uneat it.
We got to get away from eating box stuff and we got to quit eating fast food. And as I tell everybody, look, I’m a novice bourbon drinker. I love it, but I can’t overdo it. And that’s what we’re doing. We’re coming home at night. We’re stressed, we’re knocking two or three back, trying to chill. And again, now starts to dysregulate sleep, dysregulate brain function. We have to be more cognizant. Your people in a sense are cerebral athletes, but yet are fueling themselves improperly and then expecting a better result. So, diet, two.
Three, we can supplement. There are many things out there that we can take that are anti-inflammatory that also can help with producing certain chemicals in the brain and protect the brain. Fish oil is a common one. DHA and fish oil is a common one. Turmeric is a common one. It’s bigger than that. I can’t get into the list, but Lion’s Mane, the mushrooms. Adaptogens.
The list gets voluminous, but most people, that’s not what we’re doing. So, anything we can do to improve the health of our brain improves our health overall, which prevents this as opposed to just, we’re going to run down the road and see what happens.
Four, physical activity. And I know they don’t want to hear this because I don’t have time to fit that in. So, I tell all my clients, if you want to be healthy, I need 37 minutes of your life a day. Okay. Tell me what this means. Thirty minutes.
Drew McLellan:
It’s a very specific number.
Dr. Gerry Farris:
Drew, I have played with this one over and over. And that’s why I came up with 37 because when you look at your life, you can give me 37 minutes. I’ve been doing this a while. So, 30 minutes of intentional physical, that could be a walk. I watched a webinar and they said, “All doctors should write a prescription for something called forest bathing.” Okay. What is forest bathing? It’s called taking a walk in the woods and smelling the pine and listening to the birds and looking at the squirrels and turning off and tuning out.
The hippies were right on this one. Forest bathing. Simple. But again, it can be a walk. It can be some stretching. If you want to go lift weights, fine. You want to take a two or three-mile run, fine. You want to get on a Peloton, fine. But we have to rejuvenate ourselves. The body is made to move so we do need some physical activity. The seven, because I know you’re waiting for the seven.
Drew McLellan:
Right.
Dr. Gerry Farris:
The seven is intentionality of stress reduction. Okay. This is, I need you to sit and be, and turn off and tune out. This can be meditation. This can be breathing exercises. For those that are spiritual, this can be prayer, could be reading the Bible. I’ve had ladies that work in Rose Garden. But it’s just this idea that I’m going to tune out everything. And it’s hard for us. It’s incredibly hard for us. But you have to start to build this into your life every day.
And I know everyone, your listeners, is telling me, “I’m not doing seven minutes of freaking meditation. This guy’s a quack.” I’m not asking you. Start with two.
Drew McLellan:
Or don’t meditate. Do something else.
Dr. Gerry Farris:
Do something else. But be open to it because we can now start to show the studies that when we tune out and when we have this me time, we heal. How many times, and I’ll present this, how many times, if you worked on a project and you never could figure out the answer and you went to sleep and you woke up and there’s the answer. And you wonder, “Well, how did that happen?”
Drew McLellan:
Yeah. Well, that’s why everyone talks about the big ideas happening in a shower.
Dr. Gerry Farris:
Right. It’s the same thing. We’ve assimilated all this data and we can allow the machinery of the brain to do what it needs to do. But if we continue to, here we go, more data, more this, more that, we can’t decipher. We can’t function the way we’re supposed to function. So, 37 minutes a day, guys and girls. I know it seems impossible. And I guarantee you, when you start it, you’re going to hate every second of it. But embrace it. It’s taken me many years to, and still, I’m not great at it, but it doesn’t stop me from doing it.
Drew McLellan:
Right. It sounds incredibly simple. Sleep better, eat better, move. Take your seven minutes of quiet, whatever for you that is. And yet most of us don’t do any of it.
Dr. Gerry Farris:
Right. Guess what? First thing in the morning. And it’s on.
Drew McLellan:
Yeah. You’re right.
Dr. Gerry Farris:
So, this is how I tell people, just do the experiment with me for a week or two, where you don’t turn on your phone first thing in the morning. You go get your cup of coffee and you sit in your office and you don’t turn anything on. And see how that works for you.
Drew McLellan:
And if anybody dies. In your world, people die. In our world, we’re not saving lives. So, you get into your phone or your email 30 minutes later, probably nothing horrible is going to happen.
Dr. Gerry Farris:
It’s still there. It’s not going anywhere. And again, what we’re trying to do is promote positive chemical reactions in the brains. We continue to heal the brain from the assimilation of all of this input that’s happening every day.
Drew McLellan:
And the consequence of not doing any of this at best is you’re not as healthy. You’re going to stay stressed. You’re going to stay grumpy. You’re going to stay, feeling that extra weight. But what I’m hearing you say is the real consequence is not only your physical health, that your mental health is going to continue to decline.
And you did say some scary things like Alzheimer’s and Parkinson’s. I think anybody who has had a family member with dementia, that’s their greatest fear. So, are there ways for us to navigate the stress that is thrown at us every single day?
Dr. Gerry Farris:
Yeah. There are ways for us to navigate. Okay. But again, for us to do this work, we now have to, again, organize how we’re going to do this, and you all are really good at this. But we’re not doing it. We’re just not doing it. We’re just running down the road, hoping for an outcome. And what I’m telling you is that I continue to see what happens when high functioning people, and I start to see more and more of this. And they come in and it’s like, “Well, I just don’t understand.”
Well, I’m not asking what has been building up, and you just reached the pinnacle and now it’s caused you some health consequence, whatever that health consequence might be. So, what I’m really preaching to you is let’s work on being better, men, women, leaders, by taking care of ourselves.
Drew McLellan:
Yeah. We show up better for our people. We show up better for our families. Show up better for ourselves.
Dr. Gerry Farris:
Right. The mantra of let us be better. And then, that resonates to our people. Because they see, this guy’s a true leader. Nobody wants to follow a bad leader in the battle.
Drew McLellan:
So, I know you’re working with patients every day on this stuff and they’re failing miserably. So, how do you help somebody stay on course? So, like you said, if you can’t meditate for seven minutes, do it for two. Or if you can’t pick the weeds for seven minutes, do it for a minute. How do you help your patients who come back to you and go, “I’m trying, but I’m not moving the needle the way I want to.” What encouragement or what tricks or what boundaries do you help them set so that they… because all of this sounds a lot like it’s going to take a while to create the new habit.
Most of us have lived our whole adult lives, not doing any of these things with the consistency that we should. So, now you’re telling a 30 or 40 or 50 or 60-year-old, “Okay, you got to get on a different track here.” So, how do you help your patients actually do it? Because I know everybody’s listening and going, “Yes. I know I should sleep better. I know I should eat better. I know all the things, but.” And then, they have the list of buts.
Dr. Gerry Farris:
So, here’s what I tell people. First of all, psychology tells us that it takes 42 days to begin to develop a habit. It takes 84 days to make that habit stick. And I guarantee you, all of us are going to make mistakes in the first 42. Acknowledge that we’re not going to be perfect because most of us unfortunately live in the perfectionistic world. So, one is realize you’re human and you’re not going to do this perfectly. Do the best you can. The more you indoctrinate, the better you do. On days you have more time, spend more time on yourself. Avoid frustration, which can lead to the eff its.
Because if I don’t get results, well, it doesn’t work. No, it works. It’s just, now, it’s taking us 30 and 40 years to walk into the woods. I can’t walk you out in a week. And it’s not a penicillin shot, so I can’t cure your strep throat in 48 hours. So, it’s the acknowledgement that can I get organized.
Do I want to be a better man? Do I want to be a better woman? Do I want to be a better leader and organize the importance of that into my life? Because this gets sadly overlooked until there’s a crisis.
Drew McLellan:
To your point, when there’s the heart attack or the whatever, some of that’s not repairable anymore.
Dr. Gerry Farris:
Again, what I try to do is coach. Embrace it, realize you’re not going to be good at it. Get yourself organized, do what you can. And then, periodically, do some spot checks and go, “How am I really doing?” Ask someone else, am I a better leader? Get a system of checks and balances. Somebody you can confide in. And then, I always say, work with somebody on it. You don’t have to work with me per se, but get somebody in your organization go, “Can we do this together because we’re better together than we are apart?”
Drew McLellan:
For many of the listeners, one of the greatest things about owning your own business is you’re not accountable to anybody. And one of the most dangerous things about owning your own business is you’re not accountable to anybody. So, you’re exactly right, buddying up and being accountable and having a shared experience and somebody that you have to look in the eye and at least acknowledge I did or didn’t do it is a good thing. We don’t have very much of that in our lives.
Dr. Gerry Farris:
An accountability partner. And pick an accountability partner that you would not normally pick.
Drew McLellan:
How come?
Dr. Gerry Farris:
Because if you are exactly the same person on exact same level, right? So, you need to pick someone that’s a little different, that’s going to see you through a different light. And that’s a novel idea for most people.
Drew McLellan:
It really is. Birds of a feather flock together.
Dr. Gerry Farris:
When I went through it, I had to ask my daughter. I’m like, “How am I doing?” I could ask my colleagues, it didn’t mean as much. I could ask my wife and it was still rhetoric. But you ask your kids and you’re like, “Is dad being better? Am I a better man to you? Am I a better father? Am I a better leader at work? Am I a, et cetera, go on. It’s a different idea and it’s way out your comfort zone. And that’s exactly what I’m trying to get you to do.
Drew McLellan:
It would force you to humble yourself in doing it.
Dr. Gerry Farris:
Again, we have to start to look in the mirror, and that’s the hard part for all of us is that there’s so many people come see me and they walk out or they’re in tears and I’m like, “Just do the mirror test, take it all in for 48 hours and then let’s start fresh.” The mirror test is always the toughest one.
Drew McLellan:
Well, we live in a world where everything is instantaneous and again, we want to take a pill or get a shot and be all better. And this is not that, unfortunately. So, I know one of the other things you do with your clients is you help them have coping mechanisms for managing the stress that comes into everybody’s life.
Are there two or three of those that are ones that you would think, if you’re a business owner and you’re running on high octane all the time, other than what you said, which was take the break, give your brain time to heal, or is that managing stress? I know that does help you manage stress, but are there some other tips and tricks to managing the stress that’s coming at us 24/7?
Dr. Gerry Farris:
No. What you don’t want is the quick fix. We want to keep you off medication. Everybody wants what’s the fastest way to A to Z and this is not one that we should go fast from A to Z on. Then it’s, I got this and I’m going to be working on this the rest of my life. That’s the only trick is realize what I’m asking you to embrace as a lifestyle for the rest of your life. Not just for six weeks or 12 weeks or whatever. Again, it’s just embracing the idea that I really need to take care of myself. Because we’re not.
Drew McLellan:
We’ve scared the listeners for the last hour.
Dr. Gerry Farris:
I’m sorry.
Drew McLellan:
No, no, no, no. So, what I’m looking for… no, this is why I wanted to have the conversation. What do you see in the patients that follow this advice that actually do the hard work of weaving this into their lives? What changes for them?
Dr. Gerry Farris:
They become happy.
Drew McLellan:
That’s a novel concept.
Dr. Gerry Farris:
Happiness is lost in our society. They’re less stressed. They start to do this thing that we have lost, called the enjoyment of life.
Drew McLellan:
We all deserve that. Right?
Dr. Gerry Farris:
We’ve worked hard. Why are we not enjoying life? Why are we not-
Drew McLellan:
Well, and again, most of the people listening, they have a good life. They have a good family. They’re making a good living. They have all of the things that should allow them to enjoy life.
Dr. Gerry Farris:
So, a great piece of wisdom I heard the other day, because I’d had a bunch of hard days. And I play a little golf and I talked to my golfing buddy, because it took me 60 years to finally play in the old man’s golf game. It’s really fun because I’ve always, even when I was a kid as a caddy, I always wanted to play in this game. So, I’m asking these guys, so like big boy questions. That’s what we’re talking about. We’re doing big boy questions.
And we’re asking this, and the guy looks at me and he goes, “You don’t need to be an Eagle Scout anymore because you’re already an Eagle Scout. Now, I want you to sit back and ponder that for a second. We got the badge.” There’s no more badges to get. And really, guys and girls, think about this one because it resonates. And it was a simple term. We don’t need to be an Eagle Scout than we are now, but yet we continue to raise the bar when the bar is, we are the bar.
Drew McLellan:
That’s really spot on, you’re right. We’re always pushing for more. We’re pushing for more all the time.
Dr. Gerry Farris:
We are the bar. Accept it. We’re there. We’re good. There’s not much more beyond, the view is beautiful. We’re not going to get too much higher on the mountain without killing ourselves.
Drew McLellan:
Literally. Yeah.
Dr. Gerry Farris:
It’s figuratively and literally. We know that, right? Enjoy the view. We’re up there.
Drew McLellan:
This has been eye-opening, which I knew it would be. So, I’m really grateful that you spent the time with us and slapped us around a little bit to get us to think about this differently. Because I think it’s one of those things where nothing you’ve talked about isn’t something that everybody wouldn’t say, “Yes. I’m going to do that down the road or I’m going to make time for that.” And you let life push it down the road and it gets to a point where people run out of road.
Dr. Gerry Farris:
That’s what we’re trying to avoid. Don’t kick this can down the road. And just remember, we’re not going to do this march or walk perfectly. One of the great Chinese Proverbs is, “A journey of a thousand miles starts one step at a time.” Are you willing to make one step? And if you stumble, are you willing to make another step?
Drew McLellan:
Now, the consequences are pretty significant if you don’t. Right?
Dr. Gerry Farris:
I see the consequences. Again, my job is to give you awareness of what’s really going to go on because I’ve seen it. If it scares you, well, then it should resonate with you even more deeply.
Drew McLellan:
If you recognize yourself in it. So, talk to us a little bit about how you work with people and how people can get ahold of you if they want to learn more about this. You were talking about, you can do blood work and tell folks where their body is at and all of that. So, if people want to reach out to you and want to find out more about how you work with folks like us, what does that look like?
Dr. Gerry Farris:
Yeah. So, again, I have a clinic. It’s called On Point Medicine. The easiest way to contact me is through my email, which is [email protected]. And again, we try to accommodate who we can accommodate. I’m a solo operator. So, there’s only so much of me to go around. I do work with some other people that can be also advantageous in this regard, but we’re just trying to really bring the message to others that we can do this. You’re already there. You’ve done so many big things in life, but yeah.
The telephone number to the office is 704-786-4970. I’m just outside of Charlotte, North Carolina. We do see people by telehealth across the country. Usually, it can be one visit. It’s just, we talk about what we need to do and we can set up plans for you. It can be ongoing care. It’s just whatever you, as the patient needs. We do personalized healthcare. I know that’s an amazing thing.
Drew McLellan:
It is.
Dr. Gerry Farris:
We personalized healthcare. Now, the problem is that insurers don’t believe in personalized healthcare.
Drew McLellan:
That’s right.
Dr. Gerry Farris:
The greatest investment you can ever make is in yourself.
Drew McLellan:
And if you’re not healthy, the rest of it doesn’t matter.
Dr. Gerry Farris:
I see it over and over, the people that follow this, they excel. It takes them a while, but you see them come in and they’re like, “I hated you, but I love you now.”
Drew McLellan:
A lot of wisdom.
Dr. Gerry Farris:
I think I’ll probably conclude with all that.
Drew McLellan:
That’s super helpful. Again, thank you so much. Thanks for sharing your own story and reminding us that this isn’t rocket science. It’s just new habits. And as you said, it starts with awareness and then chipping away at the habits until we’ve accumulated enough good habits that we can balance out all the other stuff that’s coming at us.
Dr. Gerry Farris:
Yeah. Just get out of denial. We’re good at denial.
Drew McLellan:
That we are. Gerry, this has been great. Thank you. Thank you so much for being with us. And I have a feeling people are going to be thinking about this for a long time. So, thank you.
Dr. Gerry Farris:
Please reach out. It’s been an honor to speak to you all because if we don’t start addressing this topic, we’re going to have some fallout that’s going to be pretty ugly. And I need leaders like you all to continue to be leaders. So, whatever we can do to help you be the best at what you can do is what’s important.
Drew McLellan:
All right. You guys, this wraps up an episode that I think you’re going to be thinking about for a long time. I know that I have some work to do on this. So, I too am going to be pondering this and figuring out how to find those 37 minutes. It sounds like a small amount, but I know for all of you like me, you look at your calendar and say, “Can’t be done.” Well, you know what? We got to figure out a way. So, let’s check in on each other about that.
I would love to hear from you about how you’re going to put some of this into play. And I can’t be all your accountability partner. I’m telling you that right now. But I would love to hear about how you’re doing that because I can come back in a couple of months and say, “All right, here’s what I’m hearing from people.” Because this is a common problem.
I don’t think any of you listening didn’t recognize yourself in some aspect of what he was talking about or the descriptors that he was talking about, whether it was the bumpy sleep or the waking up in the middle of the night, thinking about the meeting or the way you’re eating. Or, for a lot of you, it’s two or three glasses of wine when you get home because you just have to de-stress somehow. So, I suspect everybody recognized themselves in some aspect of today’s episode. So, let’s collectively agree that we can be better at this because I think that’s true.
All right, before I let you go, I want to say thanks for our friends at White Label IQ. They are the presenting sponsor of this podcast. Super grateful to them. They do White Label design, dev, and PPC for lots of listeners. And they are the outsource go-to web team for lots of you. So, head over to whitelabeliq.com/ami if you want to learn more about them and the work they do.
And you know what, I will be back next week with another guest, getting you to think a little differently about the work you do and the life you lead, that’s tied to that work. And in the meantime, you know how to track me down. I’m just through @agencymanagementinstitute.com.
And I am grateful for you. I’m always grateful when you come back and you listen to another episode or I bump into you at an event and you talk about an episode that you remember, that is incredibly gratifying to me. So, do not think I take that for granted. I know how busy you are. So, I am elated to be a part of your life.
And by the way, you know what? Happy to go on the walk with you or walk the dog or whatever it is. But I suspect Gerry’s going to tell you that that’s not part of your 37 minutes if you’re listening to me talk about work. So, maybe walk without me once in a while. All right, I’ll be back next week. Thanks for listening.
That’s all for this episode of AMI’s Build a Better Agency Podcast. Be sure to visit agencymanagementinstitute.com to learn more about our workshops, online courses, and other ways we serve small to mid-sized agencies. Don’t forget to subscribe today so you don’t miss an episode.